Ellicott City Smiles Blog
Busting 4 Common Myths About Gum Disease!
August 17, 2022

Do you have gums that are sore, red, and bleed easily? Gum disease is very common. In fact, approximately half of Americans over the age of 30 are suffering from gum disease at one severity or another. However, there is all sorts of misinformation floating around online, so it can be difficult to know what is reliable. Continue reading to learn about some of the most common myths out there and why they are incorrect.
(more…)Why You Shouldn’t Ignore Your Toothache
August 3, 2022

Dental emergencies can happen when you least expect them; and they often occur when it’s incredibly inconvenient! But sometimes, something like a toothache might not seem very urgent or bothersome—so is it okay to ignore it? Not at all! Here’s more from your emergency dentist about what causes toothaches and how they can lead to some pretty severe consequences if left untreated.
(more…)Can Genetics Cause Gum Disease?
July 3, 2022
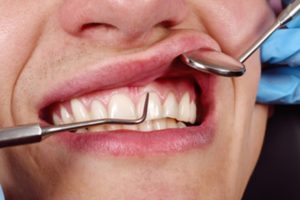
You inherit many different traits from your parents—virtually everything from your eye color to the length of your pinky toe is determined by genetics. But did you know that your genes can also leave you more vulnerable to certain medical conditions, including gum disease? Believe it or not, this condition isn’t just the result of poor oral habits! Keep reading to learn more from your dentist about how genetics can contribute to gum disease along with some tips for protecting your smile.
(more…)Gingivitis VS Periodontitis: What You Need to Know
June 24, 2022
 Did you know tooth decay isn’t the only cause of tooth loss? Gum disease is equally devastating; however, it doesn’t just affect your oral health. Research has found several connections between the preventable infection and various health issues, like cardiovascular disease, respiratory illness, and Alzheimer’s disease. Although the early signs of the infection (gingivitis) may not seem concerning, if it progresses to periodontitis, you can suffer irreversible damage. Here’s what you need to know to safeguard your health and wellness.
Did you know tooth decay isn’t the only cause of tooth loss? Gum disease is equally devastating; however, it doesn’t just affect your oral health. Research has found several connections between the preventable infection and various health issues, like cardiovascular disease, respiratory illness, and Alzheimer’s disease. Although the early signs of the infection (gingivitis) may not seem concerning, if it progresses to periodontitis, you can suffer irreversible damage. Here’s what you need to know to safeguard your health and wellness.
Is It Safe to Get Gum Recontouring?
February 17, 2022

There are numerous people out there who aren’t happy with the appearance of their smile. However, it isn’t necessarily the teeth that are always the issue. Sometimes, cosmetic imperfections can exist within the gums instead of the teeth. Fortunately, gum recontouring is an increasingly popular option to help patients achieve the smile of their dreams – but is the procedure a safe one? Continue reading to learn what gum recontouring entails and whether or not there are any risks.
(more…)A Simple Guide to 3 Common Types of Gum Grafts
January 4, 2022

Has your dentist told you that you need gum surgery to treat your gum disease? If so, you might be nervous, and understandably so. Any form of surgery can be nerve-racking, especially when you have no idea what to expect. When it comes to surgical gum disease treatments, you’ll typically undergo what’s known as a gum graft to restore the tissue that has been lost. The specifics of your procedure will vary, but here’s a general guide to three common types of gum grafts that are used to treat gum disease.
(more…)Interested in Gum Recontouring? Here’s What You Need to Know About the Cost
December 18, 2021

Are you insecure about your smile because you feel it’s too gummy? Fortunately, there is a solution: gum recontouring. In this treatment, a local anesthetic is applied to your gums before the excess tissue is carefully removed, creating a perfectly balanced smile. But what is the cost of gum recontouring? While there isn’t a flat fee, there are some factors that play a role in the price. To learn what they are, read on!
(more…)Am I a Good Candidate for Gum Recontouring?
November 4, 2021

There are many people out there who are unhappy with the appearance of their teeth. However, teeth aren’t always the issue. Sometimes, the cosmetic imperfections concern the gums instead.
Fortunately, gum recontouring is an increasingly popular option to help patients get the smile they’ve always dreamed of. But are you a viable candidate for this procedure? Keep reading to find out from your dentist in Ellicott City.
(more…)4 Cosmetic Options to Fix Small Teeth
August 29, 2021
 Teeth come in all shapes and sizes, each with their own unique beauty. Unfortunately, if you have smaller than average teeth, you might not see things the same way. It’s easy to feel embarrassed by a “gummy smile.” While you might believe it’s only an aesthetic issue, in some cases, it can compromise your oral health. You don’t need to hide your less-than-perfect smile any longer. Here are 4 ways your dentist can fix small teeth.
Teeth come in all shapes and sizes, each with their own unique beauty. Unfortunately, if you have smaller than average teeth, you might not see things the same way. It’s easy to feel embarrassed by a “gummy smile.” While you might believe it’s only an aesthetic issue, in some cases, it can compromise your oral health. You don’t need to hide your less-than-perfect smile any longer. Here are 4 ways your dentist can fix small teeth.
Can Receded Gums Grow Back?
June 22, 2021

Have you struggled with periodontal disease in the past? This is a very common issue that affects nearly half of American adults who are over the age of 30. Fortunately, it is easily preventable with proper oral hygiene and regular dental visits, but what if you have suffered with gum recession as a result. Continue reading to learn whether or not gums grow back and what you can do to ward off gum disease in its tracks.
(more…)