Ellicott City Smiles Blog
What Does It Feel Like to Have a Tooth Extracted?
April 10, 2025

Do you have a tooth extraction coming up? No one wants to get their tooth pulled; however, this procedure is sometimes necessary to preserve the health of the rest of your smile. Tooth extractions are very common, but they can sound intimidating. Read on to learn more about tooth extractions and their step-by-step process so you know exactly what you can expect.
(more…)Can You Brush Dentures While They’re in Your Mouth?
March 13, 2025

Your dentures are a durable, lifelike way to restore your smile, but just because they look and work like real teeth doesn’t mean you can always treat them like real teeth. The truth is, though your dentures will improve your ability to eat a fuller diet, speak clearly, and smile with confidence, there are still a few things you shouldn’t do with them. Here are a few things you should keep in mind to ensure that your prosthetics stay in great shape for years to come!
(more…)Why Do My Dentures Smell So Bad?
February 20, 2025
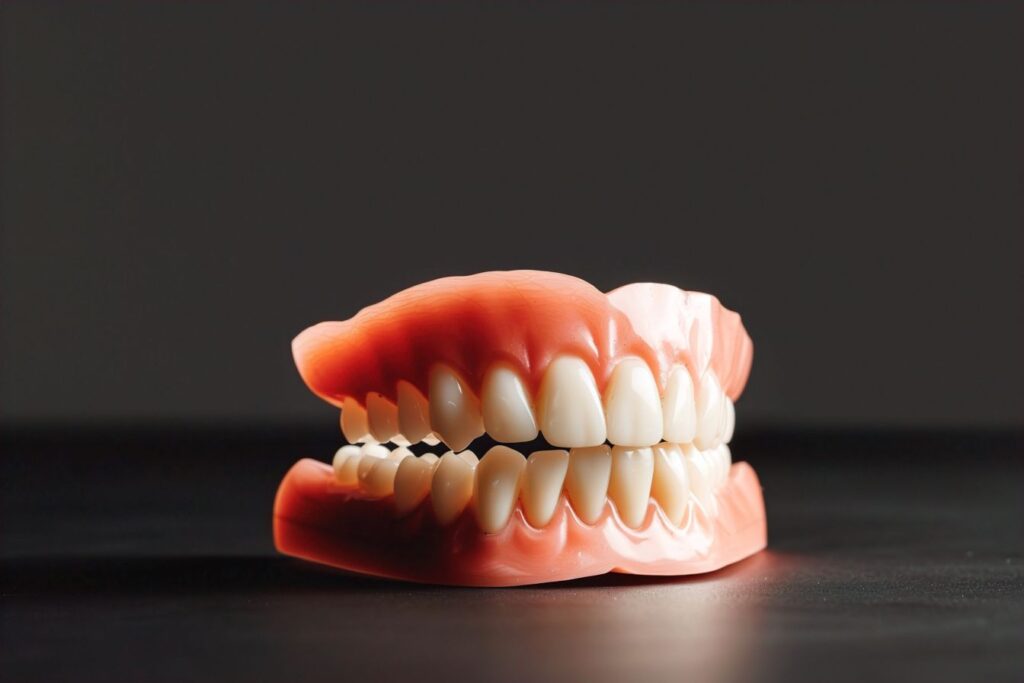
Unlike your real teeth and gums, your dentures are immune to things like cavities and infection. So naturally if you don’t brush them, it’s not a big deal, right? Wrong! The truth is, even though your dentures can’t become injured in the same way your biological teeth and gums can, they can still become damaged if you don’t take care of them. If your prosthetics have begun to smell a little foul, here’s what could be happening, and what you can do to prevent it from continuing.
(more…)Mouth Maintenance: 3 Tips to Preserve Your Dentures
January 11, 2025

Dentures are the tried-and-true way to rebuild your grin after losing some or all of your adult teeth. These versatile restorations are customized to look as lifelike as possible to simultaneously improve your mouth’s functionality and appearance. With them in place, you can eat, speak, and smile more like you used to.
Plus, dentures can last 5 to 10+ years, but you must care for them properly to continue to enjoy their many benefits. Continue reading to learn 3 ways to keep them in excellent condition!
(more…)Crossing the Finish Line: What to Expect with Braces Removal
December 27, 2024

Are you getting close to finishing your orthodontic treatment? Certainly, you can eagerly look forward to having a smile that is free of brackets and wires! But before you cross the finish line, you may want to know what you can expect with braces removal. And what will you need to do in order to maintain your results? This blog post can prepare you for the road ahead.
(more…)Myth Busters: 5 Things About Braces That Simply Aren’t True
November 21, 2024

Over the years, you may have heard things about braces – whether on social media or from TV shows. But is it true? It’s important to find out, especially regarding something as important as your oral health. Below, you will find the truth behind five popular myths about braces.
(more…)How to Survive Cold & Flu Season with Invisalign
October 17, 2024

While any time is good for Invisalign, some months are tricker for treatment than others. Patients often struggle to use the clear aligners well during cold and flu season. In fact, the winter months present unique challenges to Invisalign unless you take certain precautions. Given all those facts, your Ellicott City dentist wants to offer some crucial aligner advice. Here are four great tips on how to survive cold and flu season with Invisalign.
(more…)Back On Track! Invisalign Tips for Staying on Schedule
September 20, 2024

If you’re wearing Invisalign, you already know that consistency is vital to achieving great results. The aligners are designed to be worn for at least 22 hours a day, which can seem like a challenge when you’re juggling meals, hygiene, and everyday life. But don’t worry, it’s very possible! If you’re struggling with being consistent with your Invisalign aligners, continue reading. You’ll find some practical tips to help you meet your 22-hour wear time and get your treatment back on track!
(more…)Getting Your Dentures to Stick with Denture Adhesive
July 8, 2024

Though dentures are designed to fit pretty snug, it’s not uncommon for them to slip out of place from time to time, especially when they’re new. As the name suggests, denture adhesive can help your prosthetic stick in place. However, there are plenty of different types to choose from, all with different use instructions. It can get confusing pretty quick! Here’s what you need to know about using denture adhesive.
(more…)The Do-Over: What is Root Canal Retreatment?
June 8, 2024
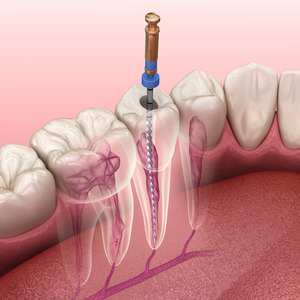
When patients see their dentist for a root canal, they’re often pleasantly surprised by what the treatment entails. Most people imagine this treatment to be lengthy and uncomfortable. However, the reality is that modern technology and powerful local anesthetics ensure patient comfort throughout the duration of their procedure.
That said, many patients aren’t exactly dying to get another root canal after their first one. In some situations, however, this is necessary. Here’s what you should know about root canal retreatment, why it’s necessary, and what the process will entail.
(more…)